This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Pt came with the complaints of
Abdominal distension since 20 days
Pedal edema upto knees since five days
History of presenting illness
Pt was apparently asymptomatic 20 days ago then she developed abdominal distension, which was insidious in onset, gradually progressive in nature
Abdominal tightness present
aggrevated after having food
Patient has pedal edema since five days- on and-off which is continuous,pitting type, upto knee level
Patient complains of SOB when abdominal bloating is present
No c/o chestpain, palpitations ,orthopnea, PND
No fever, cough, cold, vomitings ,loosestool
PAST HISTORY:
She is a k/c/o chronic liver disease since 1 yr
Pt was admitted with similar complaints 11 months back and therapeutic ascitic tap was done
K/c/o HTN since 13 years on tab Telma 40 MG PO/OD
K/c/o Hypothyroidism since13 years on tab.thyronorm PO/OD
K/c/o DM type 2 since 4 yrs on metformin 500mg PO/OD
Not a k/c/o asthma,CVA,CAD,TB,epilepsy
PERSONAL HISTORY:
Diet-mixed
Appetite:normal
Bladder movements -regular
Bowel-Has constipation
Addictions-beetelnut(pan) since 30yrs
Sleep -adequate
GENERAL EXAMINATION:
Patient was consious, coherrent and co-operative. Well oriented to time place and person.moderately built and nourished
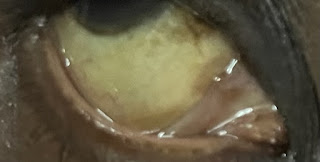
icterus -present
B/L pedal edema-present (upto knee level-pitting)
No pallor
No clubbing
No cynosis
No generalized lymphadenopathy
Vitals:
Temp: afebrile
Bp: 100/70 mmHg
PR: 72bpm
RR: 20 cpm
SpO2: 98% on RA
Systemic Examination -
ABDOMEN :
Abdomen - distended
Normal hernial orifices
Fluid thrill +
Dilated veins absent
No tenderness
No palpable mass
No organomegaly
No bruit heard
CVS :
S1 S2 + ,No murmurs
RESPIRATORY SYSTEM;
B/l symmetrical chest
Trachea - Central
B/l air entry present
NVBS heard
CMS:NFND
Investigations:
2D-echo
MRI ABDOMEN and PELVIS:
USG ABDOMEN AND PELVIS:
USG ON 6/7/23(after Ascitic tap):
Ascitic fluid sugar:187mg/dl
Ascitic fluid Protien:1.5gm/dl
Ascitic fluid for LDH:710 IU/L
Cell count of Ascitic fluid:
Total cells:100cwlls/cumm
Neutrophils:nil
Lymphocytes:100%
LFT:
Total bilurubin:3.65mg/dl
Direct bilurubin: 1.51mg/dl
SGOT: 179IU/L
SGPT: 152IU/L
Alkaline phosphate:190 IU/L
Total proteins:5.2gm/dl
Albumin: 2.84g/dl
Fasting blood sugar: 112mg/dl
Hemogram:
Hb:15.2gm/dl
TLC:10200cells/cumm
Neutrophils 86%
Lymphocytes 8%
Eosinophils 2%
MCV-89.5fl
MCH-31.3pg
MCHC-34.9%
RBC count:4.87millions/cumm
Platelets:2.39lakh/cumm
PROVISIONAL DIAGNOSIS:
Decompensated chronic liver disease ?NAFLD with k/c/o HTN and hypothyroidism since 13yrs
K/c/o DM-II since 3 yrs
HCV positive
TREATMENT GIVEN:
Fluid restriction <1L per day
salt restriction <2g/day
tab.lasilactone 20/5mg PO/OD
Syp.lactulose 10ml PO/TID
tab.telma 40mg PO/OD
tab.metformin 500mg PO/OD
tab.thyronorm 25mcg PO/OD
high Protien diet -2 egg whites/day
strict I/O charting
weight and abdominal girth monitoring
monitor vitals and inform sos
Acidic tap was done and about 600ml of fluid was removed
Pre procedure vitals:BP-100/50mmhg PR:92bpm
Post procedure:BP-120/80mmhg PR:86bpm
ADVICE AT DISCHARGE:
Fluid restriction <1L per day
salt restriction <2g/day
tab.telma 40mg PO/OD continue
tab.metformin 500mg PO/OD continue at 8am
tab.thyronorm 25mcg PO/OD continue at 8am
Tab lasilactone 20mg PO/OD x1 week at 8am
Sup.lactulose 10ml PO/TIDx1 week 8am,1pm,8pm
high Protien diet -2gm/day
FOLLOW UP:
Review to opd after 1 week










Comments
Post a Comment